What is Benign Prostatic Hypertrophy (BPH)?
Benign Prostatic Hyperplasia (BPH) is one of the most common health conditions of aging men worldwide, accounting for up to 4.5 million office visits annually. At age 70, 40% of men are symptomatic and by age 75, 50% are symptomatic.
What are the symptoms of BPH?
- Hesitancy in starting a stream
- Straining
- Prolonged voiding or weak flow
- Terminal dribbling
- Sensation of incomplete emptying
- Retention
- Overflow incontinence
- Frequency or nocturia (night time awakening to urinate)
- Urgency
- Urge incontinence
What is Prostate Artery Embolization (PAE)?
Prostate Artery Embolization (PAE) is a treatment for the condition of BPH
PAE is a minimally invasive, outpatient procedure performed through a quarter inch incision in the right grown or left wrist enabling you to return to your normal activities quickly without any risk of urinary incontinence or sexual disfunction.
Take this IPSS survey to see how severe your symptoms are. Bring it with you to your appointment to discuss your individualized treatment plan.
Why does Prostate Artery Embolization (PAE) work?
Symptoms result from an increase in size of the prostate gland, specifically the transitional zone of the gland which surrounds the urethra or "urine channel". As this multifactorial process continues in aging men, the prostatic urethra or "urine channel" becomes more and more narrow, eventually resulting in urinary retention, an inability to urinate, in some men.
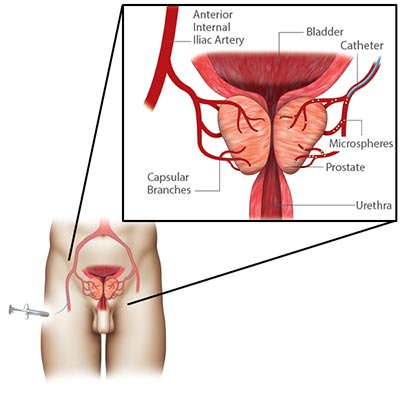
The goal of the procedure is to decrease the blood flow to the prostate gland, thus depriving the cells of the nutrients which they need to survive, resulting in cell death and an overall reduction in prostate gland size, increasing the caliber of the "urine channel" and alleviating the symptoms of BPH.
Prostate Artery Embolization (PAE) has emerged as a minimally invasive, low risk, treatment option for patients with BPH. PAE is an outpatient procedure which I perform in the Interventional Radiology fluoroscopy (live X-ray) suite with conscious sedation, also known as "twilight sleep". As general anesthesia is not required, patients with contraindications to surgical intervention may still undergo the procedure.
A multitude of medical and surgical therapies are available for the treatment of BPH, but may have undesirable side effects and complications, including retrograde ejaculation and urinary incontinence, neither of which are reported with PAE.
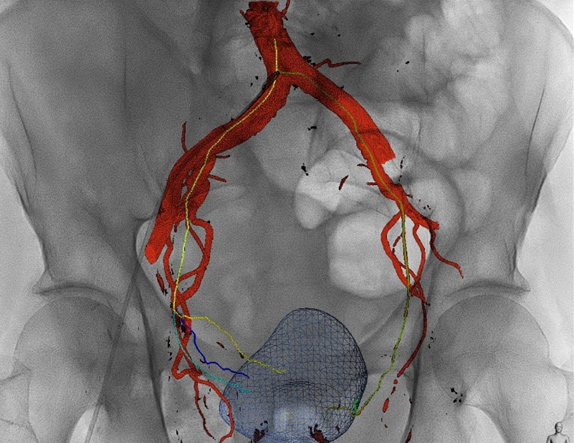
Caption: 3D reconstruction of the pelvic arteries during a real PAE procedure. The blue mesh shape towards the bottom of the image is the enlarged prostate. We have state-of-the-art technology that allows us to perform this procedure safer and faster.
How is the procedure performed?
Upon arrival in the Interventional Radiology department, an IV is started and pre-procedural antibiotics are administered to prevent infection, as well as a one-time dose of IV steroids to help decrease the inflammatory response to the embolization procedure. During the procedure, conscious sedation, or "twilight sleep" is administered by the physician and highly trained nursing personnel with continuous monitoring of the patient's vital signs.
A Foley catheter is not routinely placed. Some patients may already have a catheter in the bladder if they are dependent on one. The procedure is performed through a small, quarter inch incision in the right groin or the left wrist enabling access to the arterial system.
Specially designed wires and catheters are used to gain access into the left and then right prostatic arteries. The x-ray, or fluoroscopy, machine is used to create a specialized 3D reconstruction of the x-ray data in the form of a cone beam CT scan, to ensure access into the prostatic arteries. Small particles called microspheres less than 1 millimeter in size are delivered into the prostatic arteries, thus blocking the flow of blood into the prostate gland. Without sufficient blood supply, the cells within the prostate gland will begin to die and the gland will decrease in size over time.
Patients remain in the Interventional Radiology recovery area for approximately 3 hours post-procedure and are then discharged home. A course of oral antibiotics, a short steroid taper and high dose NSAIDs are routinely prescribed for the next seven days to prevent infection and decrease the inflammation within the prostate gland caused by the procedure.
Post-Procedure Care
In the first 3-5 days following the procedure, increased urinary frequency (up to several times per hour), bladder spasms and pelvic discomfort are common. Additional medications to decrease these symptoms may be prescribed at the discretion of the physician.
Outcomes
At approximately 4-6 weeks after the procedure the prostate gland will begin to decrease in size, thus those patients with indwelling catheters prior to the procedure may begin to undergo voiding trials.
At 6 months following the procedure an imaging study is ordered, such as a CT scan or a prostate MRI.
Success is mainly measured clinically with improved IPSS (AUA) scores but can also result in significantly increased urinary flow rates, improved bladder emptying and decreased prostate volume. An approximately 15-30% reduction in prostate gland size can occur by three months after the procedure, and up to 50% at 12 months.
In peer-reviewed literature, a clinical success rate of 88% is reported for PAE, with repeat intervention rates at 1 year equivalent to those in patients having undergone transurethral vaporization, laser resection or thermal ablation.
A randomized clinical trial including 114 patients documents equivalent symptom improvement at 6 months post procedure in patients having undergone TURP (transurethral resection of the prostate) and PAE, with equivalence remaining out to 12 and 24 months post-procedure. Of note, erectile dysfunction, and incontinence are not reported in PAE patients.
Follow-Up Care
We routinely see patients in follow-up at 3 months post-procedure for a simple ultrasound for the purpose of prostate gland measurement.
Contact Us
Interventional Radiology Clinic
Norfolk General Hospital
The physicians who perform the PAE procedure are dual-board certified in Interventional Radiology and Diagnostic Radiology. They are the only physicians in the Tidewater area who perform PAE and they received specialized training during their fellowships on PAE from one of the leading PAE centers in the US.